The jail had a perfect record. For almost 30 years, there were no suicides.
When two correctional officers rushed into Jeffrey Dugan Jr.’s jail cell at 11:30 p.m. Sunday, the streak of success was broken. He was hanging by a noose made from pieces of his mattress top. The officers lowered his body and tried to resuscitate the 33-year-old, Sheriff Brad Swain said, but the man was already dead.
Before the incident, no one suspected anything. Dugan’s fellow inmates said he seemed fine, though he had just broken up with his girlfriend.
Attempts are common in the jail setting, but since 1986, they have all been unsuccessful, Swain said. All the right steps were being taken to prevent suicides. Monroe County Jail administration even exceeded expectations when it hired a full-time psychologist to handle mental health issues in the jail.
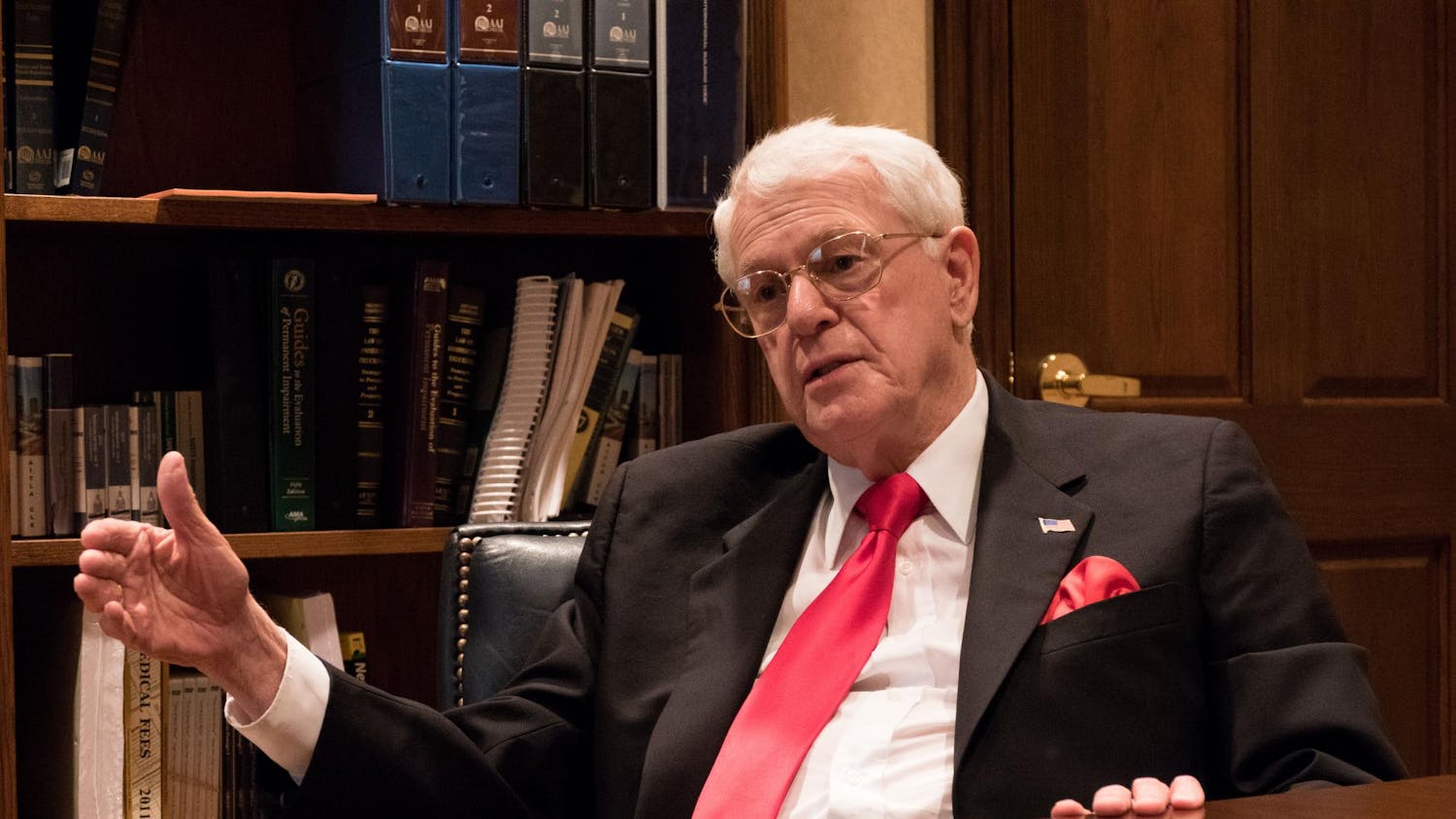
Don Weller counseled hundreds of inmates for suicide in his first year working as the jail’s counselor. Jail officers screen inmates carefully when they are booked, trying to determine who might be at risk.
But some slip through the cracks.
‘The new mental health hospitals’
Jails are intended to deter people from committing crimes, not act as mental health hospitals. But in Monroe County, now more than ever, people experiencing mental illness are winding up in jail, blurring the line between healing and punishment.
Power holders of the correctional community - the jail commander, a public defender, a circuit court judge and others - can’t pin down why they are seeing so many inmates who experience mental illness. They can’t be expected to, with no way of tracking the population, no checkbox for a jail officer to mark “mentally ill.”
Before 2013 there were routes available to jail officers when an inmate reached crisis level, but there was little the jail staff could do to manage problems on a daily basis. The Monroe County Jail commander knew something had to be done. Wary of a potential lawsuit, he found a partial fix. He hired Weller full-time.
In his first year alone, Weller saw 1,180 inmates for mental health concerns, an amount which represents about 20 percent of people booked into the jail annually.
A U.S. Bureau of Justice study found 64 percent of local jail inmates have a mental disorder, a higher rate than both state and federal prisons. Weller puts the current estimate for Monroe County between 35 and 40 percent, though he said the guess might be low.
Inmates sometimes struggle to get the prescriptions they need or think they need. Many are overcoming substance abuse. Far too often, they are not fully aware Weller can help.
“Unfortunately,” Weller said, “jails are becoming the new mental health hospitals.”
Suicide in the jail
The jail prides itself on its system of training officers, monitoring inmates and flagging people at risk of committing suicide.
Preventing suicide in jails is never easy, said Melissa Caldwell, director of mental health services for Advanced Correctional, the healthcare provider contracted for the Monroe County Jail. Suicides can happen quickly. If an inmate tries to hang himself, it takes only three minutes for brain damage and five minutes for the person to die.
“We work with such a high-risk population, the odds are against us,” Caldwell said.
Still, she thinks Monroe County excels in its progressive attitude of caring for inmates. Caldwell said it’s not uncommon for jails the size of Monroe County’s to have a suicide once a year.
Bloomington resident Daniel Cooper said he was booked into the Monroe County Jail for getting into a fight about two years ago. After a couple days in the jail’s drunk tank, Cooper said he got rowdy with the jail officers. The officers had to confine him, which landed him in a padded segregation cell.
That was when Cooper took off his socks. He tied them together and pretended to hang himself off the cell’s ceiling vent. He said he wasn’t serious about the attempt, but he spent a week in the padded cell before a nurse came to see him. They had a brief conversation — she asked him whether he intended to kill himself, and Cooper said no.
Though Weller was not on staff when Cooper was in jail, he said the staff will take suicide attempts seriously, even feigned attempts like Cooper’s.
In the two most recent unsuccessful suicide attempts, he and the medical staff did not suspect the two inmates would try to commit suicide. The first time, an inmate made a noose and then reached out for help. In the second instance, a jail officer stopped the attempt within three minutes.
Most inmates experiencing mental illness will not attempt suicide. Sometimes, it’s the people who seem perfectly healthy — people like Dugan — who the jail staff don’t realize need the most help.
The Monroe County Jail ordered an unusually high number of psychoactive drugs in 2014 compared to the previous four years. Psychoactive drugs in medicine are used to treat mental and emotional disorders. For the first time in five years the jail ordered more psychoactive medications than blood pressure prescriptions. However, some blood pressure medications can be used to treat anxiety or related disorders.
Prescribing drugs
The jail is accommodating unusually high numbers of mental health concerns, data collected by the Indiana Daily Student suggests. Last year marked a five-year high in the number of mental health-related medications ordered by the jail.
For the first time since 2010, the jail ordered more psychoactive medications than blood pressure
prescriptions.
If an inmate already has a prescription when they are booked, they should be able to get it in jail. Still, inmate complaint records show grievances about the jail’s medical services are all too common. For the past five years medical complaints were the most common grievance filed by inmates.
“I need my medicine,” one inmate wrote in 2011. “I am getting sick, headaches and weak. I will contact my lawyer soon if I don’t receive my medicine.”
Another inmate complained in 2010 he was not receiving his prescribed medications in the jail, despite the urgency of his medical situation. The inmate identified himself as having a mental health concern.
Weller said the jail usually won’t give antidepressants to someone who has never had a prescription.
Substance abuse in county jails is estimated to be as high as 90 percent. Because of this, Caldwell said care providers are encouraged to be conservative when prescribing medications for mental and emotional disorders, which are addictive in nature.
People booked into jails might appear to be battling mental illness, while in reality they could be recovering from drug or alcohol abuse. Mental illness and substance abuse often intermix.
For many, the jail serves as a stable place to detoxify and rehabilitate.
Weller knows the administration is concerned that if prescriptions are handed out, everyone will want medications they don’t have prescriptions for. He also knows the inmates with the most profound mental health problems are usually not the ones asking for medications.
If someone remembers being uncomfortable in jail, there is a better chance they won’t re-offend. But as the inmates’ counselor, Weller wonders whether offering some medication might take the edge off the frustration, sadness or anxiety someone might feel in the jail.
He did not agree with the decision to deny a prescription to a 32-year-old man who he suspects has had depression all his life.
Stereotypes of medical staffs in jails might suggest they are uncaring and reluctant to prescribe medications. But Caldwell feels most medical staffs in jails are cautious with prescriptions because most medications, even painkillers like Advil, come with serious side effects.
“We are very conscientious prescribers,” Caldwell said.
Jails can serve as places to keep people safe and help them recover from their maladies, and Weller understands the jail staff members have the difficult task of weighing peoples’ pain against their medical
necessity.
“It’s a balance between the stick and a soft landing place,” Weller said.
Identifying inmates who need help
Weller has been working in the jail for about seven years, although only one in his capacity as the jail’s full-time psychologist. In his first year, the jail has begun new methods of identifying inmates who might need help for mental health concerns.
Since April 2014 there has been a series of questions jail officers ask inmates when they are booked into the jail. The officer will fill out a survey for each inmate.
“Is Thinking about Killing Himself,” is one category. A second, “Feels That There is Nothing to Look Forward to in the Future.” Another, “Is Acting and/or Talking in a Strange Manner.”
If someone is flagged from these questions, Weller will come to see them. There are other reasons Weller will visit inmates. The medical staff might suggest it, or if they are in one of the jail’s segregation cells, commonly used for people who are sick or experiencing mental illness, he will visit them at least once a week. They can also self-request a visit.
Sometimes Weller struggles to reconcile his tendency to be the “touchy feely psychologist” and the employee of a county jail. He likes the inmates, and they usually like him.
On one occasion, an inmate even crafted a figurine of Weller’s guide dog, Lorenzo, out of toilet paper and coffee grounds. Lorenzo assists Weller, who has been confined to a wheelchair since a bike accident in 1989. The little sculpture of the doe-eyed yellow lab sits on the desk in Weller’s office.
The counselor has learned these people are on the radar of the law for some reason. Inmates come to jail because of their own decisions, he said.
Counseling a man with six or seven counts of child molestation, for example, can be a struggle. Weller sees the man once a week. He said he likes the man, but he knows he’s done some awful things.
Still, everyone deserves to be treated with dignity and respect, Weller said, and part of his job in the jail is to advocate for people who cannot advocate for themselves.
Not every person with a mental illness in the jail is going to get Weller’s help. Sometimes they don’t know he’s available. More often though, people with mental illness don’t seek out help
Slipping through the cracks
When Weller came to see Susan Lyons inside the jail, she didn’t want to see a counselor.
Lyons told the IDS she was approached by Weller during one of her short stints in the jail. Weller was not asked to comment on Lyons' situation because of patient confidentiality.
She struggles with dementia and schizophrenia, she said. Ninety percent of her memories are gone. Lyons has no recollection of some of the men she dated, and she remembers little about the last time she was arrested.
She knows the police picked her up because she was being too loud — she is frustrated about not having a home despite being sober for five years.
“I’m tired,” Lyons said. “It’s not like I’m not living in reality, I’m just pissed off.”
The pressure can get to be too much, and sometimes she has an emotional outburst. It’s then that the police show up. Lyons has been in the jail for misdemeanor charges several times in recent years.
Lyons was annoyed when Weller came to see her. She told him she didn’t need to see a psychologist. Yet she said she hasn’t seen a counselor from Centerstone, Bloomington’s behavioral healthcare provider, nor is she on any kind of prescription for her mental health concerns.
It can be hard to engage people with untreated problems like Lyons’.
Weller said the sort of people who don’t want treatment are usually the most unstable and the ones that cycle through the justice system.
The community could benefit from more resources to handle mental illnesses, said Kenneth Todd, one of Monroe County’s circuit court judges.
While Monroe County has long been perceived as a state leader in finding alternatives to deal with mental illnesses, some people — like Dugan and Lyons — have problems that never come to light.
“We’ve closed our eyes and turned our backs on the mentally ill to the point that there’s virtually no resources to deal with them, and it’s getting worse every year,” Todd said.
During the winter months, Lyons said people in the homeless community might envy those spending time in the jail. She has even thought about being loud on purpose just so she would have somewhere quiet and warm to go.
“That’s the safest place to be, is inside the jail cell,” Lyons said. “No one can get in there.”
Beyond the jail
Unless the community can do something to keep people out of trouble and get treatment for the people who need it, the reality for the jail won’t change.
Every year, county corrections has to do a little more to meet the needs of people with a mental illness who have been caught up in the law. This year they’re working on renovating storage space into a few extra cells specifically for mentally ill inmates.
As the inmates’ counselor, Weller’s role is to ensure people in the jail are getting the care they need while they are locked up. Perhaps like any psychologist, he still thinks about how his past patients are doing.
He tries to empower them to seek help outside the jail. If they do, there’s a much better chance of not coming back.
“You hope for the best and trust that they’ll find the help they need,” Weller said.
After they leave, they are out of his hands.
This article has been updated to clarify the nature of Weller's relationships with his patients, and to clarify that Weller did not speak to the IDS about Lyons.